Abstract

Introduction
Life expectancy amongst individuals with sickle cell disease (SCD) has plateaued, with cardiopulmonary complications now becoming a leading cause of death (Fitzhugh et al. Am. J. Hematology 2010). Indeed, SCD is associated with increased rates of pulmonary hypertension (pHTN) and diastolic dysfunction (Sachdev et al. Blood 2005). In the general population, atrial fibrillation (AF) is associated with an increased mortality in the setting of either pHTN or diastolic dysfunction. Although cardiac structural and biochemical changes likely create an electrophysiological substrate for AF in SCD, the prevalence and risk factors for AF in SCD remain unclear. We determined the prevalence, incidence, and clinical characteristics of AF in a large cohort of patients with SCD.
Methods
We conducted a retrospective, longitudinal cohort study of all adult patients with SCD seen at our large, urban single center from January 2008 to December 2017. SCD patients were identified using a previously described semi-automated system with a subset with direct chart review (Srisuwananukorn et al. Blood Advances 2020). We performed manual review of ~17,000 available electrocardiograms of all enrolled subjects to look for AF. For univariate analyses, the associations of linear and categorical variables with AF were assessed using the Kruskal-Wallis test and Pearson's χ 2 test, respectively. We used Bonferroni correction for categorical variables with greater than two groups. Logistic regression analysis with stepwise addition of variables (p>0.15) was used to evaluate for the effects of previously described AF risk factors, degree of anemia, hydroxyurea use, and genotype on AF development.
Results
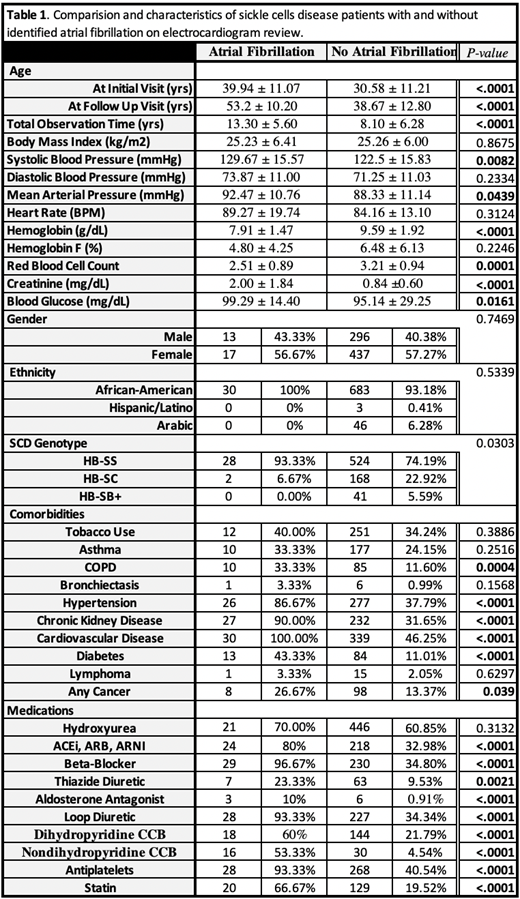
Our cohort consisted of 763 adult SCD patients with a median age of 27.95 years, 59.50% female, 72.4% with Hb SS or Sβ 0-thalassemia genotype, and 61.2% were prescribed hydroxyurea. Mean observation time for the cohort was 8.3 ± 6.3 yrs. We identified AF in 30 out of 763 adult SCD individuals with a mean age onset of 51 ± 10 years (median age 52 years). The period prevalence of AF was 3.93% and the incidence density was 3.02 per 1000 patient years observed. Individuals with AF tended to be older at initial (40 vs. 25 years, p<0.0001) and follow-up (53 vs. 35 years, p<0.0001) visits and were observed for a longer period (13.3 vs. 9.5 years, p=0.0014). There was no difference in gender (p=0.7), ethnicity (p=0.5), or SCD genotype (p=0.03) between groups (see Table 1). Those with AF were more likely to carry diagnoses of chronic obstructive pulmonary disease (p=0.0004), hypertension (p<0.0001), chronic kidney disease (p<0.0001), type 2 diabetes (p<0.0001), and any cancer (p=0.04). However, hydroxyurea use was not associated with AF development (p=0.3). SCD patients with AF were more likely to receive diuretics, atrioventricular nodal blocking agents, antihypertensives, antiplatelets, and statin therapies (see Table 1). AF was associated with worse anemia and reduced renal function. Regression analysis identified significant odds ratios (ORs) for age at initial visit (OR 1.06, p=0.03), serum creatinine per 1 mg/dL increase (OR 2.34, p=0.02), hemoglobin level per 1 g/dL increase (OR 0.52, p=0.0009), fetal hemoglobin level per 1% increment (OR 0.81, p=0.008), and total observation time per year follow up (OR 1.26, p=0.0006).
Conclusion
We showed that the prevalence and incidence of AF is high in patients with SCD with the median age of onset occurring 1-2 decades earlier than in the general populace (Feinberg et al. JAMA Internal Medicine 1995). AF in patients with SCD is associated with advanced age, worse renal function, a higher degree of anemia, and greater usage of cardio- and nephro-active medications. The high incidence of AF in patients with SCD may contribute to the plateauing of life expectancy and identifying the causative risk factors and the underlying mechanisms may not only improve life expectancy but also the quality of life. Further study is warranted.
Saraf: Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal